Non-Celiac Gluten sensitivity (NCGS) is becoming a widely discussed topic as more people report experiencing gluten-related symptoms despite not having celiac disease. Unlike celiac disease, which is triggered by an autoimmune response and has clear diagnostic criteria, NCGS remains a complex and often misunderstood condition. Symptoms commonly associated with NCGS include bloating, fatigue, brain fog, and digestive discomfort after consuming gluten, even when tests for celiac disease or wheat allergies come back negative.
If you’ve recently been diagnosed with NCGS or are exploring a gluten-free lifestyle due to persistent symptoms, this guide is here to help. We’ll delve into what NCGS is, how it affects individuals, and the practical steps you can take to manage it. Our goal is to provide clear and actionable insights, empowering you to make informed decisions for your health and well-being.
What is Non-Celiac Gluten Sensitivity?
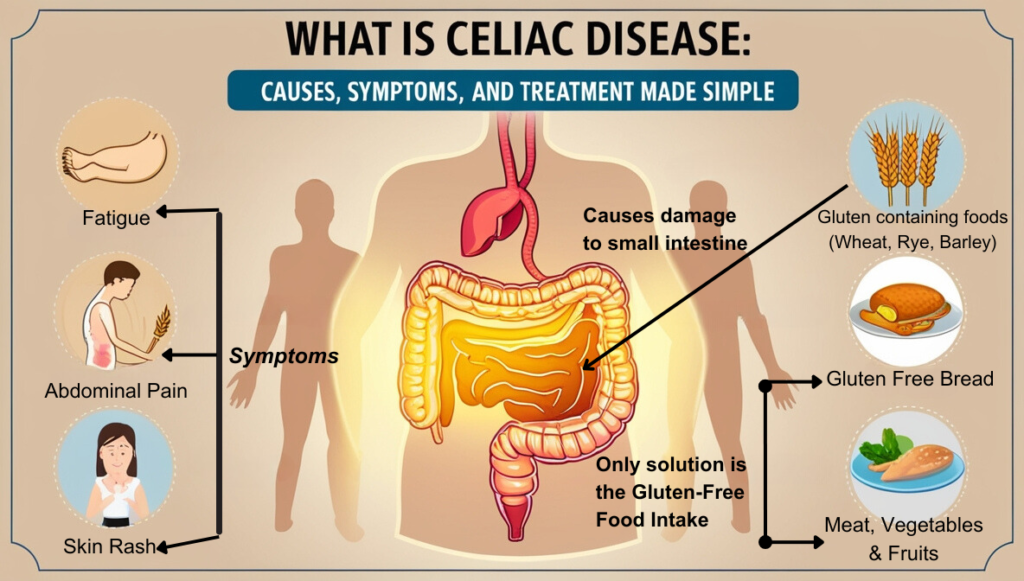
Non-celiac gluten sensitivity (NCGS) is a condition where people experience negative reactions to gluten even though they don’t have celiac disease or a wheat allergy. When someone with NCGS eats gluten-containing foods, it can trigger a variety of symptoms, but unlike celiac disease, it doesn’t cause serious intestinal damage or long-term health risks.
The exact cause of gluten sensitivity isn’t fully understood, but researchers believe it may involve an immune response to certain components of gluten or other compounds found in wheat, barley, and rye.
The symptoms of gluten sensitivity can vary widely. Some people may experience mild symptoms like bloating, fatigue, or headaches, while others may face more severe issues such as joint pain, brain fog, or digestive discomfort. These symptoms can also change between episodes, making it challenging to pinpoint gluten as the exact cause.
If you suspect gluten intolerance or sensitivity, it’s important to track your symptoms and consult a healthcare professional for guidance.
Symptoms of Non-Celiac Gluten Sensitivity
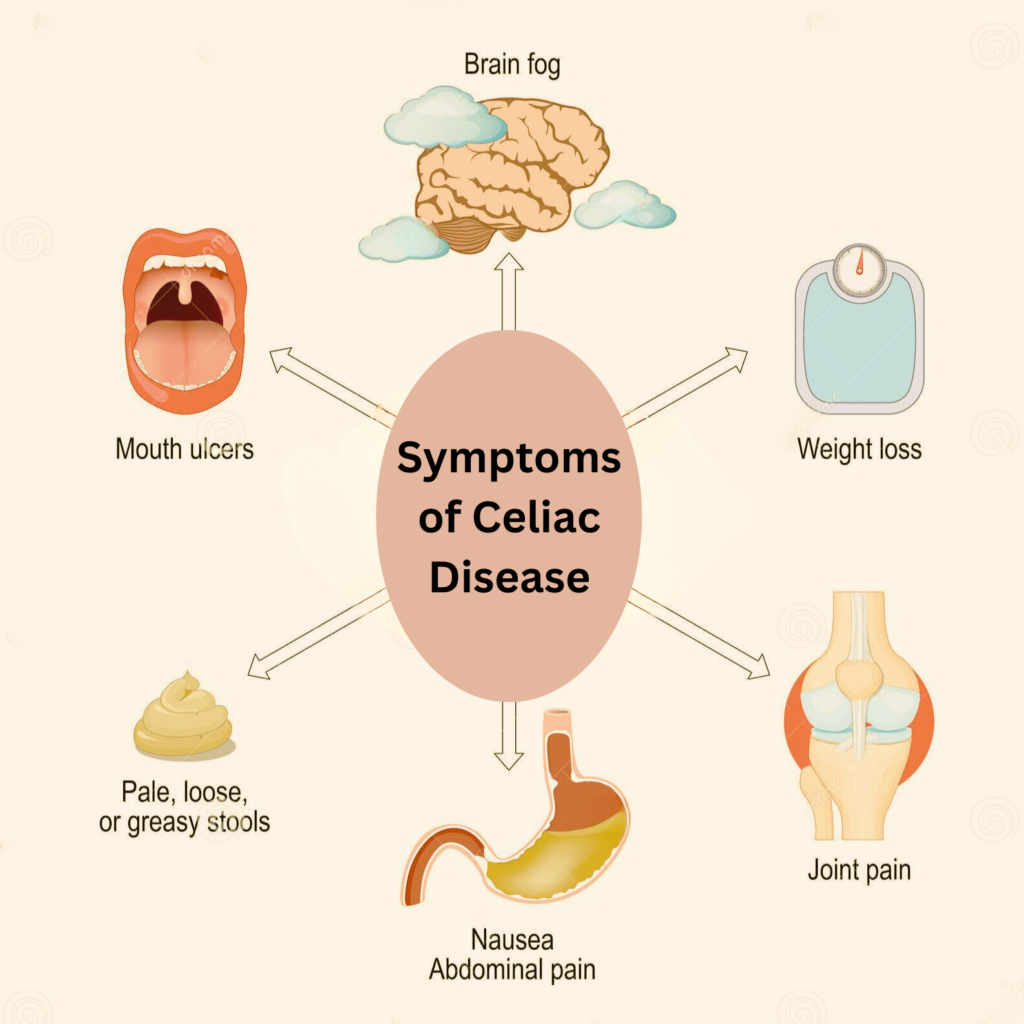
NCGS is characterized by symptoms almost similar to those of celiac disease symptoms but without the immune-mediated destruction of the small intestine or the presence of specific antibodies. Individuals with NCGS might experience:
Gastrointestinal Symptoms of Non-Celiac Gluten Sensitivity
Gastrointestinal symptoms are among the most common challenges faced by individuals with NCGS. Ranging from mild discomfort to intense pain, these symptoms can profoundly disrupt daily life. It’s not unusual for those with NCGS to experience these issues after consuming gluten.
Abdominal Discomfort
Abdominal discomfort can manifest as pain or a general uneasy feeling in the stomach area.
Bloating
Bloating is common, where individuals might notice their abdomen feels swollen or tight after consuming gluten.
Diarrhea or Constipation
Diarrhea or constipation can occur, with some people experiencing one or the other, or alternating between the two, leading to irregular bowel movements.
Similarity to Other Disorders
These symptoms often mimic those of irritable bowel syndrome (IBS) or other digestive disorders, but in the context of NCGS, they resolve when gluten is removed from the diet.
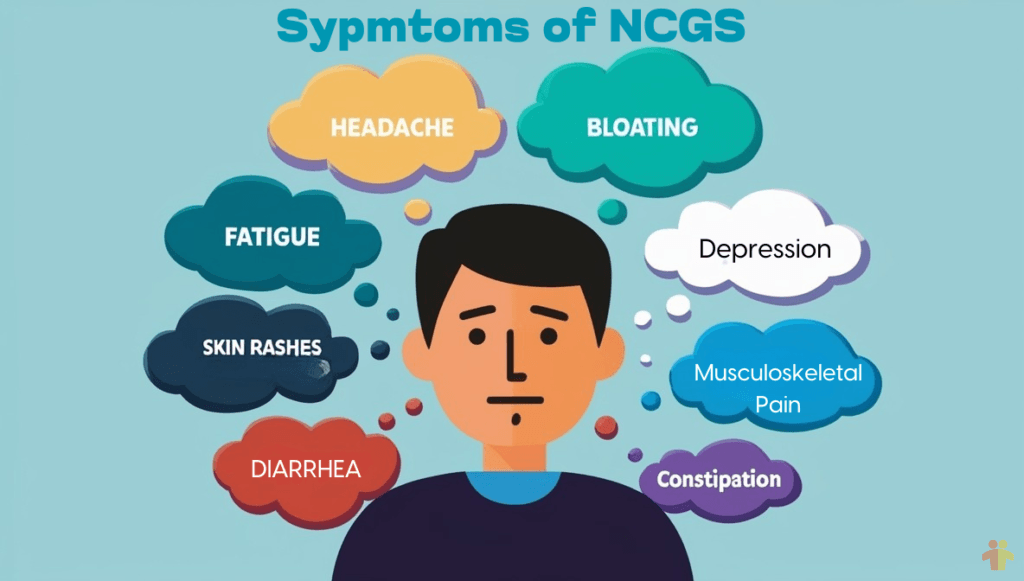
Non-Celiac Gluten Sensitivity Symptoms Beyond the Gut
In addition to gastrointestinal symptoms, some individuals may experience non-gastrointestinal symptoms such as fatigue, brain fog, headaches, joint pain, and skin rashes. These symptoms may seem unrelated to digestion but can result from inflammation caused by consuming gluten.
Fatigue
Individuals might experience profound fatigue, making daily activities challenging.
Headaches
Headaches can range from mild to severe, possibly disrupting normal routines.
Cognitive Impairment
Often described as “brain fog,” this involves difficulties with concentration or memory.
Musculoskeletal Pain
Musculoskeletal pain might manifest as joint or muscle aches.
Skin Eruptions
Skin rashes or dermatitis can develop unexpectedly and without an obvious cause.
Mood Disturbances
Mood challenges like depression can occur, contributing to emotional difficulties.
These symptoms indicate that NCGS impacts various body systems beyond the digestive tract and tend to improve once gluten is removed from the diet.
Diagnosing NCGS: A Process of Elimination
The diagnosis of Non-Celiac Gluten Sensitivity (NCGS) often involves a process of elimination. Doctors rule out conditions like celiac disease and wheat allergies before identifying NCGS. Recognizing the symptoms and knowing the diagnostic process can provide clarity on how gluten may be affecting your health.
Rule Out Celiac Disease
This process typically involves serological testing, where blood tests check for specific antibodies like anti-tissue transglutaminase (tTG) and anti-endomysial antibodies (EMA), which are markers of celiac disease. If these tests are negative, a biopsy might still be performed to examine the small intestine for any signs of damage characteristic of celiac disease. If no damage or specific antibodies are found, celiac disease can be ruled out, paving the way to consider NCGS as a possible diagnosis.
Exclude Wheat Allergy
To exclude wheat allergy when investigating Non-Celiac Gluten Sensitivity (NCGS), healthcare providers typically conduct allergy tests such as skin prick tests or blood tests for IgE antibodies specific to wheat proteins. These tests can identify an immediate allergic reaction to wheat, which would manifest symptoms like hives, itching, or anaphylaxis shortly after wheat consumption. If these tests come back negative, indicating no wheat allergy, it helps narrow down the diagnosis to NCGS, as the symptoms are not due to an allergic response to wheat but potentially to gluten or other components in wheat.
Gluten-Free Diet Trial
This involves a period where the individual strictly avoids all gluten-containing foods to see if their symptoms resolve or significantly improve. If symptoms indeed disappear or lessen during this gluten-free phase, gluten is then deliberately reintroduced into the diet to observe if the symptoms return. This re-emergence of symptoms upon gluten reintroduction helps confirm that gluten is likely the cause of the individual’s discomfort, supporting a diagnosis of NCGS.
Challenges in Research of Non-Celiac Gluten Sensitivity
Research into Non-Celiac Gluten Sensitivity (NCGS) faces considerable challenges, including issues with trial design, inconsistent symptoms, and difficulties in maintaining dietary compliance. These obstacles hinder the ability to conduct definitive studies and establish clear diagnostic criteria for NCGS. Several theories have been proposed:
Absence of Reliable Biomarkers
Diagnosing Non-Celiac Gluten Sensitivity (NCGS) presents significant challenges due to the lack of specific biomarkers. Unlike celiac disease, which can be definitively identified through blood tests for specific antibodies and intestinal biopsies, NCGS offers no such clear diagnostic tools. This absence complicates the process, often leaving clinicians to rely on indirect methods like dietary elimination trials. As a result, diagnosing NCGS becomes less straightforward and more susceptible to misinterpretation.
The Placebo Effect
The placebo effect plays a significant role in studying non-celiac gluten sensitivity (NCGS). In many trials, participants report feeling better on a gluten-free diet—not necessarily due to an actual sensitivity to gluten, but because they believe in the diet’s benefits. This psychological response can distort research findings, making it challenging to differentiate genuine cases of NCGS from perceived improvements linked to dietary changes. Consequently, proving the existence and prevalence of NCGS becomes more complicated, requiring meticulously designed studies to minimize the influence of placebo effects.
The Role of FODMAPs
The role of Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols (FODMAPs) adds an additional layer of complexity to what is often diagnosed as Non-Celiac Gluten Sensitivity (NCGS). Wheat, in addition to containing gluten, is also rich in these short-chain carbohydrates, which can trigger digestive discomfort in some individuals. Research indicates that a low FODMAP diet—naturally low in gluten—can alleviate symptoms in those diagnosed with NCGS. This overlap raises the possibility that, for certain individuals, symptoms attributed to gluten may actually stem from FODMAPs. This challenges the view of NCGS as exclusively a gluten-related condition, encouraging further exploration of other dietary factors.
The Immune Response
Non-Celiac Gluten Sensitivity (NCGS) differs from celiac disease in that it doesn’t trigger the same autoimmune response. However, research suggests the immune system may still play a role, though to a lesser degree. Studies have found that individuals with NCGS experience elevated levels of specific cytokines—molecules that signal inflammation—after consuming gluten. This indicates that gluten can provoke an inflammatory response, contributing to their symptoms, even though it doesn’t cause the intestinal damage associated with celiac disease.
The Gut Microbiota
The gut microbiome may play a critical role in non-celiac gluten sensitivity (NCGS). Consuming gluten has the potential to disrupt the balance of gut bacteria, triggering changes that could lead to symptoms in individuals sensitive to gluten. While research in this area is still emerging, scientists are investigating how gluten impacts the gut’s microbial communities and its possible contribution to symptoms like bloating, abdominal pain, and discomfort in NCGS patients. Gaining a deeper understanding of this interaction could pave the way for new strategies to manage or even prevent symptoms by targeting gut health.
Living with Non-Celiac Gluten Sensitivity
Living with Non-Celiac Gluten Sensitivity (NCGS) involves navigating dietary restrictions, symptom monitoring, and nutritional considerations. The cornerstone of management is a gluten-free diet, although some may benefit from a low FODMAP approach. Vigilance in tracking symptoms and ensuring balanced nutrition is essential for a healthy life with NCGS.
Dietary Management
The primary approach to managing Non-Celiac Gluten Sensitivity (NCGS) involves adopting a gluten-free diet, which means eliminating wheat, barley, rye, and sometimes oats from one’s intake. This dietary shift can lead to symptom relief for many, but it’s not without its challenges, as gluten is prevalent in many processed foods. Moreover, for some individuals, a low FODMAP diet might prove more beneficial. This diet restricts fermentable carbohydrates that can cause digestive issues, including those found in wheat. While potentially more effective for symptom control, a low FODMAP diet is significantly more restrictive, requiring careful planning to ensure all nutritional needs are met.
Monitoring Symptoms
Living with NCGS often necessitates vigilant symptom monitoring. Keeping a detailed food diary can be invaluable; it allows individuals to track not only when they consume gluten but also to identify other dietary triggers that might exacerbate symptoms. Symptoms can vary widely from person to person, making it essential to recognize personal patterns. This practice can help in fine-tuning the diet, possibly extending beyond just gluten avoidance to include other potential irritants or intolerances, thereby enhancing quality of life through better symptom management.
Nutritional Considerations
Switching to a gluten-free diet can inadvertently lead to nutritional shortfalls if not managed properly. Gluten-free products often lack the fortification found in their gluten-containing counterparts, potentially leading to deficiencies in fiber, iron, calcium, and B vitamins. Consulting with a dietitian is crucial to navigate these challenges. A dietitian can provide guidance on selecting gluten-free foods that are nutrient-dense, suggest alternatives to ensure a balanced diet, and recommend supplements if necessary. This professional support helps maintain health while adhering to the dietary restrictions imposed by NCGS.
The Social and Emotional Impact
The lifestyle changes required for managing Non-Celiac Gluten Sensitivity extend beyond mere dietary adjustments, significantly impacting social interactions and emotional well-being. Individuals with NCGS might find themselves excluded from social events centered around food, leading to feelings of isolation or the need to constantly explain their dietary restrictions, which can strain relationships. Emotionally, the vigilance needed to avoid gluten can contribute to heightened levels of stress, anxiety, or even depression, as the fear of symptom flare-ups can be ever-present.
However, the establishment of strong support networks, whether through family, friends, or NCGS support groups, can offer substantial psychological relief. These networks provide a sense of community, understanding, and shared experiences, which are crucial for coping with the emotional toll of the condition, helping individuals maintain a positive outlook while navigating life with NCGS.
Current Research and Future Directions
Current research into NCGS focuses on genetics, microbiome interactions, biomarker discovery, and refining trial protocols to enhance understanding and management.
Genetic Studies of Non-Celiac Gluten Sensitivity
The exploration into the genetic underpinnings of NCGS is a promising avenue for future research. By identifying specific genetic markers or predispositions, scientists could not only better understand why some individuals react to gluten without celiac disease but also tailor dietary advice more precisely to those at risk or diagnosed with NCGS. Such genetic insights could lead to more personalized management strategies, potentially reducing the broad spectrum of dietary exclusions to those truly necessary for each individual.
Microbiome Research of Non-Celiac Gluten Sensitivity
Research into how gluten influences the gut microbiome offers another frontier in understanding NCGS. The gut flora plays a crucial role in digestion, immunity, and overall health, and alterations in this microbial environment might be key to why gluten causes symptoms in some people. By delving deeper into these interactions, researchers hope to uncover mechanisms through which gluten affects the microbiome, potentially leading to novel therapeutic approaches that could restore microbial balance, reduce symptoms, or even prevent NCGS in susceptible individuals.
Development of Markers Non-Celiac Gluten Sensitivity
The ongoing quest for specific biomarkers for NCGS would be a game-changer for diagnosis. Currently, the absence of clear markers leads to a reliance on dietary trials, which can be cumbersome and subjective. Discovering biomarkers would not only simplify and speed up the diagnostic process but also help in monitoring the condition and assessing the effectiveness of dietary interventions. This could lead to more definitive treatments and a better understanding of the condition’s impact on various body systems.
Better Trial Protocols
Improving the design of clinical trials for NCGS is crucial for obtaining clearer, more reliable data. The sensory differences between gluten-free and gluten-containing foods, the variability of symptoms, and the challenge of dietary compliance have historically complicated these studies. Enhanced protocols could involve better methods for blinding, more precise symptom tracking, and innovative ways to ensure adherence to dietary restrictions. Such improvements would not only clarify the prevalence of NCGS but also elucidate its mechanisms, potentially leading to better management strategies and less reliance on broad dietary exclusions.
Conclusion
Non-Celiac Gluten Sensitivity remains a complex and somewhat elusive condition, but continued research and improved understanding are vital for individuals struggling with its effects. In the meantime, maintaining a gluten-free diet while seeking support from healthcare professionals, loved ones, and the NCGS community can help mitigate its impact on daily life. With ongoing research into genetics, microbiome interactions, biomarkers, and clinical trial protocols, there is hope for better management strategies in the future. Until then, vigilance and support remain crucial for managing Non-Celiac Gluten Sensitivity effectively.
Lastly, it’s important to remember that NCGS is a real and valid medical condition that can significantly impact an individual’s quality of life. It’s essential to offer support and understanding to those living with NCGS, as they navigate the challenges of managing their health while adhering to a gluten-free diet.
By staying informed and advocating for more research, we can work towards a future where individuals with this condition have access to better diagnostic tools, treatment options, and improved quality of life.