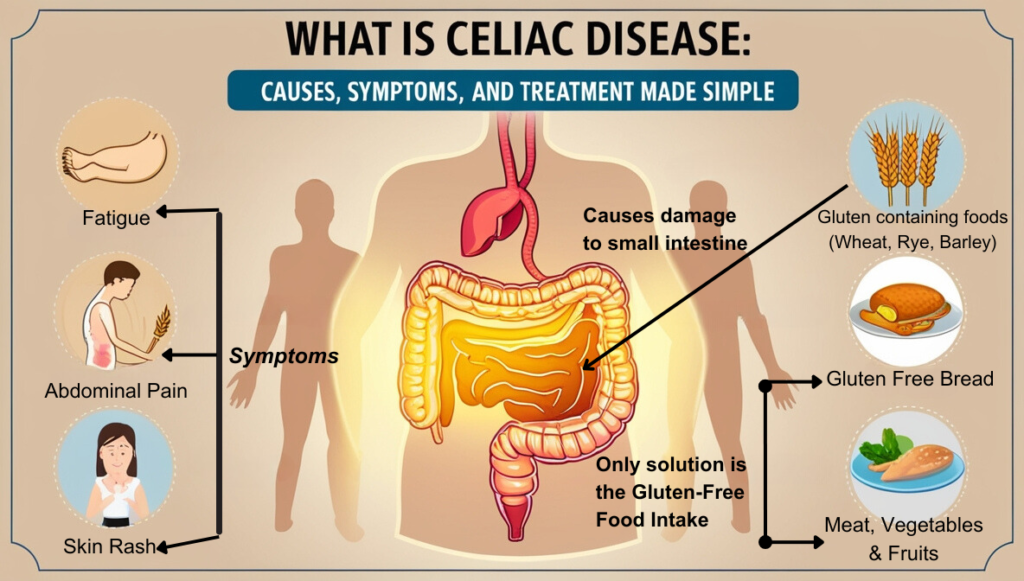
Celiac Disease is a serious autoimmune disorder where the human immune system attacks the small intestine upon consuming gluten (a protein in wheat, barley, and rye). The protein damages the intestine’s lining and hinders nutrient absorption. If left untreated, it can cause long-term health complications.
The questions as to who does it affect?
What causes celiac disease in the first instance?
How can it be diagnosed and treated?
And most importantly – why is it important to understand the celiac disease?
This guide aims to answer all of these questions for you in a simplified and easy-to-understand format.
What is Celiac Disease?
Celiac Disease is a chronic condition of the digestive system. The term “Chronic” refers to a long-lasting state of health that persists over time and may never go away.
With Celiac Disease, the immune system reacts against gluten keeping your body from digesting food properly.
The villi, tiny finger-like projections in your intestine that aid nutrient absorption, get damaged in the process. When Villi becomes less effective at absorbing nutrients, vitamins, minerals etc , malnutrition eventually sets in.
And it is the malnutrition that causes people with celiac disease to experience a wide range of symptoms like fatigue, bloating, diarrhea and even depression.
So it is imperative to understand the symptoms first to treat this disease in a proactive manner.
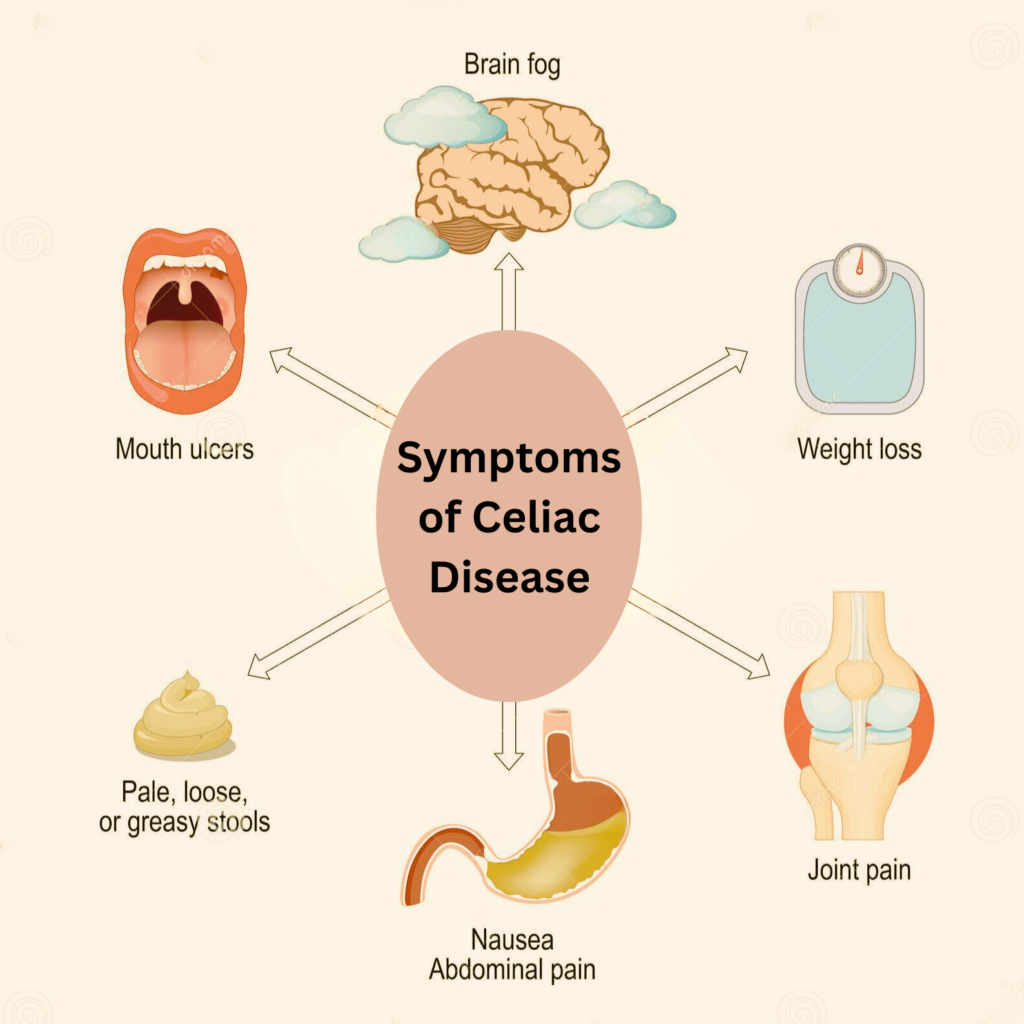
Identifying Symptoms of Celiac Disease
Once we know what to look out for, we can identify the symptoms of celiac disease.
1. Digestive issues
Finding yourself constantly dealing with bloating, gas and diarrhea?
It could be a sign of celiac disease. These digestive problems occur as a result of the body’s inability to properly digest gluten.
People also report experiencing constipation, abdominal pain and nausea. For some, these symptoms may only occur occasionally, while for others it can be a chronic issue.
2. Skin rashes or irritations
Dermatitis herpetiformis is a skin condition when people develop itchy, blistering rashes. These lesions stem from their body’s immune reaction to gluten. If you have recurring skin irritations, it could be a sign of celiac disease.
Lupus, Psoriasis and Eczema find an association with Gluten Intolerance. However, only a medical professional can confirm if it is celiac disease or not.
3. Joint pain and inflammation
Swelling and stiffness in joints such as the knees, hips, fingers and wrists occur in people with celiac disease. Gluten triggers the body to produce inflammation. At times, if the inflammation is severe, it can cause joint damage.
Gout and arthritis get a boost from celiac disease.
4. Fatigue and weakness
Feeling constantly tired may indicate anaemia, often caused by iron deficiency. Celiac disease can lead to anaemia due to poor nutrient absorption.Women may experience fatigue more than men. Mental fatigue, difficulty in concentrating and low energy levels drench patients of celiac disease.
Some patients report an extreme fatigue that could be a sign of Chronic Fatigue Syndrome associated with gluten intolerance.
5. Nutritional deficiencies:
Since celiac disease affects the body’s ability to absorb nutrients, people with this condition may suffer from nutritional deficiencies. Common deficiencies include iron, calcium, and Vitamin D.
As we know, calcium and vitamin D are crucial for maintaining healthy bones. Hence celiac disease patients may have a higher risk of developing osteoporosis.
What Causes Celiac Disease?
After understanding the symptoms, it is essential to know what causes celiac disease. While scientists are still researching the exact cause of this condition, there are some known factors.
1. Genetic Factors
Celiac disease has a strong genetic component, meaning it can run in families.
If you have a first-degree relative (parent, child, sibling) with the condition, your chances of having it increase to 1 in 10. The HLA-DQ2 and HLA-DQ8 genes are associated with celiac disease and are present in about 30% of the general population.
However, having these genes does not necessarily mean you will develop the disease.
2. Environmental Triggers
While genetics may predispose someone to celiac disease, it is not the only factor at play. Research indicates that certain environmental triggers can activate or worsen the condition.
Gluten Exposure
The primary environmental trigger for celiac disease is the consumption of gluten-containing foods at a young age. Studies suggest that introducing gluten between 4 and 6 months, especially in predisposed infants, can affect the likelihood of developing celiac disease.
Researchers also believe that the amount and frequency of gluten consumed by the infant can play a role in the development of the disease.
Infections
People who are more likely to get celiac disease need to keep a close watch on their stomach health. Infections, like Gastroenteritis, often referred to as stomach flu, can make symptoms worse and even start celiac disease in those who are prone to it.
So, it’s important to pay attention to stomach health and see a doctor quickly if there are any issues.
Gut Microbiome
The gut microbiome refers to the balance of microorganisms in the digestive tract. Research suggests that imbalances in gut bacteria may contribute to celiac disease.
Studies have shown that individuals with celiac disease have lower levels of beneficial bacteria and higher levels of harmful bacteria in their gut. This imbalance can make symptoms worse for those with celiac disease.
Stressful Life Events
Significant physical or emotional stress, including surgery, trauma, or childbirth, has been associated with triggering celiac disease in predisposed individuals. These events may disrupt immune function or alter the gut environment, setting off the disease.
Diagnosis and Testing Methods
If you suspect that you or a loved one may have celiac disease, it is crucial to seek medical attention for proper diagnosis and treatment. The diagnostic process typically involves multiple steps:
1. Medical History and Physical Exam
The first step in the diagnostic process is discussing your symptoms with a doctor and providing them with a detailed medical history. Symptoms such as digestive issues, skin rashes, and nutrient deficiencies can help a doctor determine if celiac disease is the likely cause.
Your health practitioner may exam you physically to check for any signs of malnutrition or anemia.
If they suspect , they will move on to the next step.
2. Blood Tests
Gluten intolerance triggers the body to produce specific antibodies that can be detected through blood tests. The most common test used to diagnose celiac disease is the tissue transglutaminase IgA (tTG-IgA) test.
If this test comes back positive, your doctor may order additional blood tests to confirm the diagnosis.
3. Biopsy
Small intestine biopsy remains the gold standard for diagnosing celiac disease.
This procedure involves taking small tissue samples from the lining of the small intestine and examining them under a microscope for damage or inflammation caused by gluten.
4. Genetic Testing
If someone has positive blood test results and negative biopsy results, their doctor may suggest genetic testing to confirm whether they carry the HLA-DQ2 or HLA-DQ8 gene associated with celiac disease.
Siblings and children of individuals with celiac disease may also undergo genetic testing to determine their risk.

Core Treatment Options for Celiac Disease
At present, there is no known cure for celiac disease, and the only effective treatment is to follow a strict gluten-free diet. This means avoiding all foods and products that contain gluten. People with celiac disease must eliminate even trace amounts of gluten from their diets as it can trigger symptoms and cause damage to the small intestine.
Following this diet can help heal the small intestine and improve symptoms such as digestive issues and skin rashes.
There are many benefits to following a strict gluten-free diet for people with celiac disease. These include improved nutrient absorption leading to alleviation of nutritional deficiencies, reduced risk of complications such as osteoporosis, and improved overall quality of life.
In addition to dietary changes, there are other potential treatments that may be recommended by a doctor to manage symptoms of celiac disease. These include:
1. Vitamin and Mineral Supplements
Nutritional deficiencies are common in people with celiac disease, and supplements can help replenish any nutrients that may be lacking due to dietary restrictions. These supplements often include vitamins D, B12, iron, and folate.
2. Medications
Some medications may be prescribed by a doctor to manage specific symptoms of celiac disease. For example, anti-diarrheal medication can help control digestive issues, while topical creams or ointments may alleviate skin rashes caused by gluten intolerance.
Practical Solutions for Managing Celiac Disease
Being diagnosed with celiac disease can initially feel overwhelming, but with proper treatment and management, leading a healthy and fulfilling life is entirely possible. Effective management of celiac disease demands commitment and practical strategies. Here are some practical solutions for those diagnosed with this condition.

1. Educate Yourself About Gluten
Hidden sources of gluten hinders a gluten-free diet. Edible and non-edible items such as medications, vitamins, and even makeup can contain gluten. So it is essential to read labels carefully , research nearby restaurant menus, and cross-contamination risks.
2. Join a Support Group
Joining a support group can provide significant emotional and practical assistance . These groups create a safe space where individuals share their experiences, challenges, and victories, fostering a sense of community and belonging.
Members exchange tips on managing a gluten-free lifestyle, such as safe food products, cooking techniques, and eating out. Additionally, support groups often provide educational resources and invite guest speakers, such as nutritionists or health professionals, to talk about the latest research and advancements in celiac disease management.
3. Empower Yourself in Social Situations
Eating out or attending social events can be daunting for someone with celiac disease. However, it is crucial to speak up and advocate for yourself by asking questions about ingredients and food preparation methods.
4. Have an Emergency Plan
Being prepared for accidental gluten exposure is vital for those living with celiac disease. Keeping medications on hand to manage symptoms and having a plan in place for emergency situations can help prevent any serious health complications.
5. Choose Alternative Grains
Eliminating wheat, barley, and rye from your diet may seem challenging initially. However, there is an abundance of alternative grains available such as quinoa, buckwheat, amaranth, and rice that are safe for celiac disease patients.
6. Cook Meals at Home
Preparing meals at home allows you to have complete control over the ingredients used in your food. It also reduces the risk of cross-contamination from other sources.
Get creative and experiment with new gluten-free recipes to keep your meals exciting and enjoyable.
Conclusion
In conclusion, understanding what celiac disease is, how to identify its symptoms, and what causes it can help individuals take necessary precautions and improve their quality of life.
While a gluten-free diet is currently the only treatment for celiac disease, early diagnosis and management can prevent long-term complications and ensure a healthier future for those living with this chronic condition.
It’s important to consult with a healthcare professional if you suspect you or someone you know may have celiac disease, as only a medical diagnosis can confirm the condition. With proper management and support, individuals with celiac disease can lead fulfilling and healthy lives.
So, it is essential to educate ourselves and raise awareness about this widespread yet often misunderstood condition. Remember, knowledge is power, so let’s use it to make a positive impact in the world of healthcare.